A Simple Overview
Have you ever dealt with nagging liver issues, gallbladder problems, or even gut troubles like Crohn’s disease—but you’re still searching for answers? If so, the PEMT gene could be the missing puzzle piece. PEMT stands for phosphatidylethanolamine N-methyltransferase, but don’t let that long name scare you. Simply put, PEMT helps your body make phosphatidylcholine (PC)—a crucial “building block” that keeps your cells and your digestive system healthy.
What Is Phosphatidylcholine (PC)?
Phosphatidylcholine might sound fancy, but it’s basically a type of fat that’s vital to your body:
It Builds Healthy Cell Membranes
PC is one of the main ingredients in the walls (membranes) that surround every cell in your body. Think of it like the “bricks” that protect each cell.It Keeps Your Liver Lean and Happy
Your liver uses PC to “package” and ship out fats so they don’t pile up and cause fatty liver issues.It Helps Your Gut Lining Stay Strong
A special coating in your intestines needs enough PC to keep gut bacteria at a safe distance. This can be extra important if you deal with Crohn’s disease, ulcerative colitis, or other digestive concerns.
So, PC is a big deal.
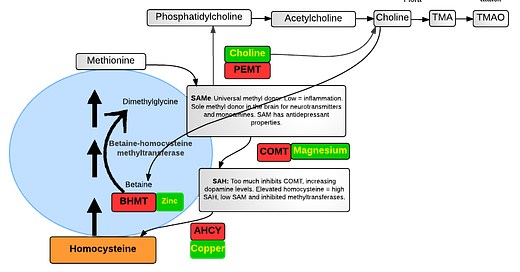
How PEMT Fits In
Most of your PC might come from the foods you eat (like eggs or sunflower seeds), but your body has a Plan B in case you don’t get enough from your diet: the PEMT pathway. With the help of PEMT, your liver can make its own phosphatidylcholine from other ingredients.
However, if you have genetic variations (sometimes called “mutations” or “SNPs”) in the PEMT gene, your liver may have trouble producing PC. In other words, you rely more heavily on your diet to supply it. For some people, that can lead to:
Fatty liver disease or elevated liver enzymes
Gallbladder problems (like gallstones)
Inflamed gut issues (Crohn’s, ulcerative colitis)
Why the Gut Connection?
Ever wonder how a genetic quirk in your liver can affect your gut? Here’s the scoop:
Your colon has a protective mucus layer that’s rich in phosphatidylcholine.
If you don’t have enough PC (due to a sluggish PEMT gene or a poor diet), this mucus barrier weakens.
That allows gut bacteria and toxins to irritate the lining of your intestines, leading to inflammation.
Studies show that giving extra PC to people with ulcerative colitis can help reduce symptoms and encourage healing of the gut lining. Pretty amazing, right?
How to Support a Sluggish PEMT
Focus on Choline-Rich Foods
Foods like egg yolks, liver, and sunflower lecithin are great sources of choline, which your body can convert into PC. If you’re vegetarian or rarely eat these, consider a choline supplement.Consider Phosphatidylcholine Supplements
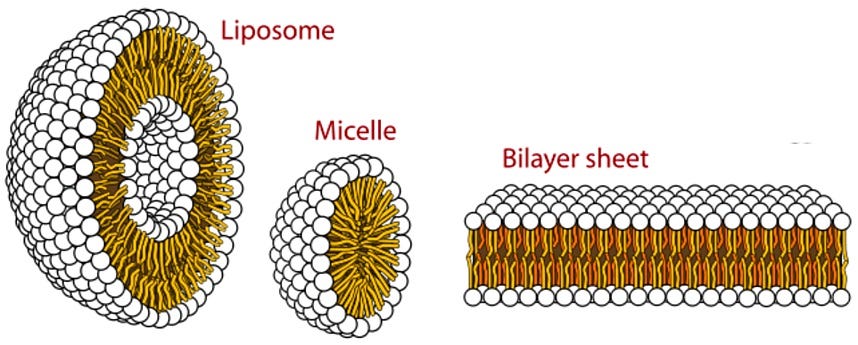
Many find that adding a direct PC supplement (often made from soy or sunflower) helps their liver and gut. Look for “phosphatidylcholine” or “lecithin” on the label.Don’t Forget Glutathione
Glutathione is your body’s main antioxidant. A special form called liposomal glutathione also delivers extra phosphatidylcholine (since it’s wrapped in tiny PC bubbles). Some products, like VARS Glutathione, combine both benefits—protecting your cells and giving you a PC boost.Probiotics & Fiber
If you’ve had gut issues like Crohn’s or colitis, a high-quality probiotic (e.g., Natren Healthy Trinity) can support a healthier balance of gut bacteria while you rebuild that PC-rich mucus barrier.Test, Don’t Guess
If you suspect a PEMT mutation might be at play, genetic testing can confirm it. Then you’ll know for sure if your body struggles to produce PC on its own.
Putting It All Together
The PEMT gene is more than just a random snippet of DNA—it’s a key player in your liver health, gut function, and even your overall energy levels (healthy cells mean better energy!). If you’ve had mysterious liver enzyme elevations, gallbladder issues, or chronic gut inflammation, it could be worth investigating your PEMT status.
Remember: No single strategy fits everyone. Some folks do great just by eating more eggs and taking a daily choline supplement. Others might need a phosphatidylcholine supplement or a glutathione product. The big takeaway is to give your body enough phosphatidylcholine—whether that’s through diet, supplements, or both.
Next Steps for Better Health
1. Talk to a Knowledgeable Provider: Share your concerns about PEMT with a functional medicine or integrative practitioner who can guide you on testing and supplementation. You can ALWAYS reach to my practice and we can work with you from ANYWHERE.
2. Check Your Diet: Sneak more choline-rich foods into meals.
3. Explore Supplemental Options: If needed, add a phosphatidylcholine or liposomal glutathione product to your regimen.
4. Keep Monitoring: Watch how your liver markers, digestion, and energy respond. Adjust with the help of a professional.
By tuning in to your PEMT gene and ensuring you have enough phosphatidylcholine, you just might unlock better digestion, a healthier liver, and a more resilient body overall.